As my luck would have it, I posted a positive video update to my facebook page last Sunday afternoon feeling really pleased and excited that I was about to finish my four week dose of 24/7 IV antibiotics. My inflammatory markers had gone right down, meaning that after almost nine months of ongoing infection and a bout of sepsis, it was looking like we finally had this pesky infection under control.
 Photo: me just a couple days ago! Would you see me in the street and think that girl has cancer?
Photo: me just a couple days ago! Would you see me in the street and think that girl has cancer?
With the infection being under control, my appetite has finally returned and I have regained a couple kilos, which is a good sign for me considering I lost at least 10kg’s post-surgery.
I still have daily pain and need to take regular pain relief, but considering the level of pain I had just a few short months ago, it has definitely improved and isn’t so debilitating. Touch wood. Lets not jinx myself with this now too!
Lately I’ve had people telling me how well I look, which is great, because I love not looking so deathly pale and fragile. However, I decided to write this blog post to help educate people that not everyone’s exterior is a reflection of their interior. Don’t get me wrong, I am glad I “look” well and healthy, but in this world of social media, you only see what I want you to see.
Invisible illness! That’s what they call it, when on the outside it looks like there is nothing wrong, but on the inside, it’s a whole different story. If I were to show you my CT scans, you would see the true mess that is going on inside.
 Photo: me about a month ago. Yes there’s some visible weight loss if you knew me pre-cancer, but other than that, nothing really to worry about here hey? Think again 😦
Photo: me about a month ago. Yes there’s some visible weight loss if you knew me pre-cancer, but other than that, nothing really to worry about here hey? Think again 😦
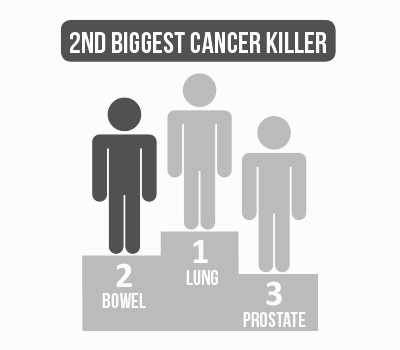
There are many different types of invisible illness: depression, anxiety, PTSD, fybromyalgia, lupus, to name just a very few! Mine? Crohn’s Disease and Bowel Cancer. All that has happened to me (and continues to do so) is mostly all internal. Sure I have plenty of surgical scars, that are hidden underneath clothing and that I am not at all ashamed of, they are proof that I am far greater than whatever tried to kill me! And yes you can see the weight loss, the pale lifeless skin, the sad eyes and lack of energy, but that’s nothing a pretty outfit and make-up can’t fix, as well as a good old fashioned belly laugh! I was lucky enough to not lose my hair so I didn’t look like your “typical cancer patient”. You would have no idea what is going on inside this body of mine – and I don’t blame you, nor do I expect you to, because even I find it hard to grasp the fact that I can look seemingly well on the outside, but on the inside it’s a completely different story.
 Photo: I was battling infection here!
Photo: I was battling infection here!
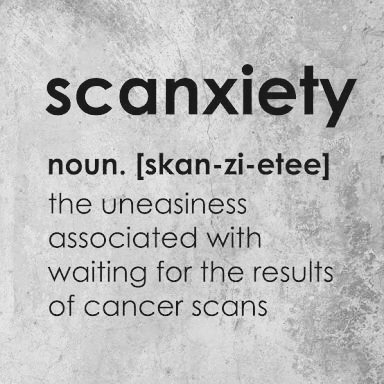
It is somewhat soul destroying, to think that you are doing well because you are looking well, and sometimes even feeling well, to have really promising blood results, to feel as though you are finally improving, only to be told that no – nothing has improved, at all… well, not internally anyway. After 32 sessions of intensive hyperbaric oxygen therapy and four weeks attached to IV antibiotics 24 hours a day, 7 days a week, the internal cavity (aka my open wound) has not improved even slightly. It is still open, a big vacant space where the tumour used to be, and still at high risk of becoming infected and turning into sepsis again. Because it was exposed so early on to such serious infection, it just seems to be refusing to heal. There is also a lot of internal “thickening” or “thickened masses” that they don’t know whether it’s cancer or not.
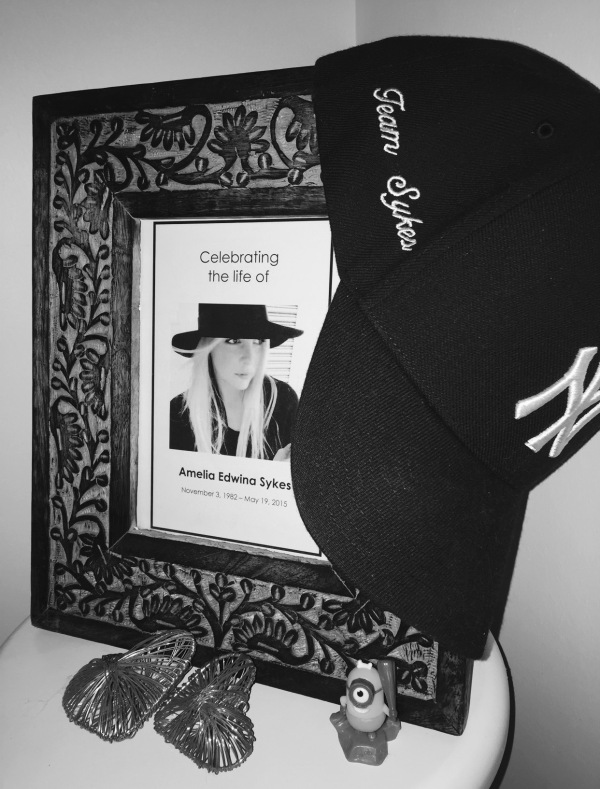
It’s really just a “watch and wait” scenario now. I am continuing the IV antibiotics for another four weeks, and once the new hyperbaric chamber at the new hospital is up and running, I will complete my oxygen therapy. I am focussed on creating happy memories, doing what I can when I can, indulging in self pampering and just taking life one day at a time.
It is hard, really hard, knowing I don’t look sick on the outside, but also knowing on the inside my body is working against me. Every single photo in this blog post, is me with cancer, fighting infection, fighting pain, fighting fatigue. It’s an eye opener, but it’s reality. People are always fighting battles you may know nothing about, and battles that may not be visible, however I choose to be open about this, with hope that I will help educate and create a better understanding.
 Photo: me just yesterday, enjoying an incredibly happy moment with my sister, niece & nephew for my niece’s birthday. Memories to cherish!
Photo: me just yesterday, enjoying an incredibly happy moment with my sister, niece & nephew for my niece’s birthday. Memories to cherish!


 Photo: Me with gold medallist and swimming superstar Kyle Chalmers at the event I organised. In this photo, despite knowing I had cancer again and was facing more major life-altering surgery, I still managed to smile, I was proud of myself for powering through!
Photo: Me with gold medallist and swimming superstar Kyle Chalmers at the event I organised. In this photo, despite knowing I had cancer again and was facing more major life-altering surgery, I still managed to smile, I was proud of myself for powering through!